Evaluation of a New ICU Environment
VITALITY, A prospective observational cohort study
Published
Delirium is one of the most frequently seen brain organ dysfunctions in the intensive care unit (ICU). Depending on the ICU population, up to 87% have delirium at some point during their critical illness. Patients with delirium have a 3fold increased risk of dying compared to patients without delirium.
Studies show that sedation is one of the most common independent risk factors for transitioning to delirium. However, a no-sedation approach is often challenging: ICU patients often suffer from symptoms of severe anxiety and agitation. One of the primary reasons for the development of anxiety and agitation in critically ill patients is the ICU environment itself. The feelings of being constantly surveyed by monitors and being exposed to different machinery or equipment are significant stressors.
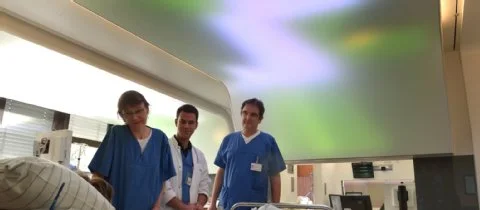
Together with our project partners ART+COM and GRAFT Architects we developed a ICU room concept to reduce patients' anxiety, helplessness, and stress. The patient's perceptions and needs were the starting point of this project. Besides the interventions aimed at noise shielding and the change of workflow, we conducted modifications to improve lighting conditions: One integral part of the room is a new light ceiling for each bed that extends from the head above the patient down to the patient's feet and covers an area of 15 square meters.
“… But what I see these days are paralyzed, sedated patients, lying without motion, appearing to be dead, except for the monitors that tell me otherwise.”
The purpose of the prospective proof of concept pilot study was to investigate if a multicomponent change in ICU room design, including light therapy, prevents delirium in mechanically ventilated patients. Second, the influence of lighting conditions on serum melatonin was assessed. Additional information regarding the study protocol can also be found at ClinicalTrials.gov. The clinical examination included a prospective assessment for depth of sedation, delirium, and pain every 8 hours using validated scores. Blood samples for serum melatonin profiles were collected every 4 hours for a maximum of three 24-hour periods.
Study Flow Diagram. 0, day of patient enrollment; SMAP, Serum Melatonin Assessment Period (A, 1st day of intervention; B, 3rd day of intervention or later; C, 5th day of intervention or later.); SCP, Sedation Check Period; RASS, Richmond Agitation Sedation Scale. Numbers in yellow squares indicate the time of blood plasma collection for melatonin assessment (e.g., 8 = 08:00 in the morning). Figure published in Critical Care Medicine
Seventy-four patients were included in the analysis. Seventy-six percent (n = 28) of patients in the standard rooms developed delirium compared with 46% of patients (n = 17) in the modified rooms (p = 0.017). Patients in standard rooms (vs. modified rooms) had a 2.3-fold higher delirium severity (odds ratio = 2.292; 95% CI, 1.582–3.321; p < 0.0001). Light intensity, calculated using the measure of circadian effective irradiance, significantly influenced the course of serum melatonin (p < 0.0001). Significant interactions (p < 0.001) revealed that differences in serum melatonin between patients in standard and modified rooms were not the same over time but varied in specific periods of time.
In conclusion, modifications in ICU room design may reduce delirium, where dedicated light therapy potentially contributed to differences in outcome. For additional key information and figures regarding the study results, kindly visit our blog post.